Large body of evidence suggests that hypoxia drives aggressive molecular features irrespective of cancer type. Non-Hodgkin lymphomas (NHL) are the most common hematologic malignancies characterized by widespread disease and frequent involvement of diverse hypoxic microenvironments (e.g., bone marrow, malignant effusions, large lymphoma masses). Impact of long-term hypoxia on the biology of lymphoma cells and its potential role in mediating drug resistance and disease relapses due to adaptive changes shaped by the hypoxic microenvironment remain only partially understood.
In this study we analyzed impact of short- and long-term hypoxia on a panel of six lymphoma cell lines including diffuse large B-cell lymphoma (UPF4D, UPF8D), Burkitt lymphoma (Ramos, UPF9T), and mantle cell lymphoma (HBL2, MINO). Only 2 out of 8 tested lymphoma cell lines (Ramos, and HBL2) survived longer than 4 weeks under deep hypoxia (1% O2). The remaining tested lymphoma cell lines died by hypoxia-induced apoptosis (which could be inhibited by co-cultivation with pan-caspase inhibitor Z-VAD-FMK).
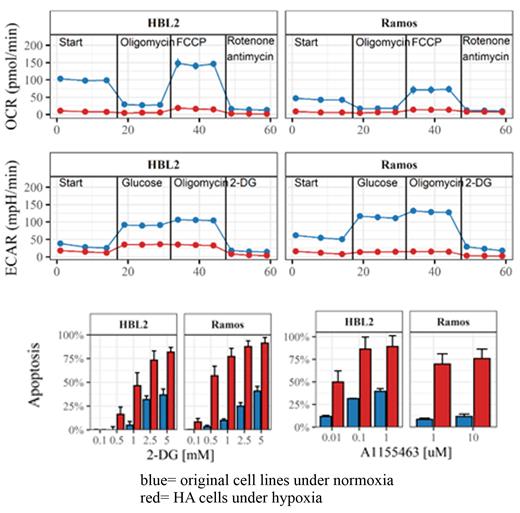
The hypoxia-adapted (HA) Ramos and HBL2 cells had severely decreased proliferation rate accompanied by complex changes of the transcriptome, proteome, and metabolome. Seahorse analysis revealed significant inhibition of both oxidative phosphorylation and glycolytic pathways ( Figure 1). Of note, the whole-proteome profiling confirmed significant downregulation of proteins regulating oxidative phosphorylation, but significant upregulation of proteins regulating glycolysis. Sensitivity of HA cells to 2-deoxyglucose, an inhibitor of glycolysis was markedly increased ( Figure 1). The data suggest that under long-term deep hypoxia, lymphoma cells try to compensate for the decrease in ATP production from the oxidative phosphorylation process by boosting structural machinery of glycolysis, on which they became vitally dependent for survival. Despite the increased glycolytic machinary, however, the level of glycolysis decreases due to severe lack of oxygen. In our opinion, this is a clear representation of the Warburg effect, a hallmark of cancer based on the metabolic reprogramming of the cancer cells under hypoxia.
Sensitivity of HA cells to a panel of the tested cytotoxic drugs (cytarabin, cisplatin, bortezomib) and targeted agents (venetoclax, S63545, A1155463, TRAIL, polatuzumab vedotin, IM-156, copanlisib) was either unchanged or increased (compared to sensitivity of the original cell lines cultured under normoxia). In contrast to so far published data, long-term hypoxia was not associated with acquired drug resistance in case of any of the tested agent. Of note, HA cells became significantly more sensitive to A1155463, an inhibitor of anti-apoptotic protein BCL-XL ( Figure 1). Unchanged levels of BCL-XL protein in HA cells and the respective normoxic cell lines (detected by western blotting) suggest that more complex mechanisms plausibly underlie the observed markedly increased sensitivity to A1155463.
The whole-transcriptome and proteome analyses of both HA cell lines (compared to the parental cell lines cultured under normoxic conditions) detected among other complex changes signficant upregulation of P4HA1 (both mRNA, and protein), a prolyl hydroxylase involved in the stabilization of hypoxia-induced factor (HIF) 1 alpha, and putative oncogene associated with tumor aggressiveness. Transgenic (over)expression of P4HA1 in hypoxia-sensitive MINO cells effectively inhibited the hypoxia-induced apoptosis. Western blot analysis implemented on a panel of primary lymphoma cells revealed markedly higher expression of P4HA1 protein in the lymphoma cells obtained from malignant effusions (putative hypoxic microenvironment) compared to lymphoma cells obtained from leukemized blood (putative normoxic microenvironment). Our data suggest that P4HA1 positively impacts survival of lymphoma cells under hypoxia.
In translation, P4HA1, BCL-XL, and structural proteins of the glycolytic pathway may represent novel drugable targets for more effective elimination of hypoxia-adapted lymphoma cells.
Financial Support: Ministry of Health of the Czech Republic AZV NU23-03-00172, Grant Agency of the Czech Republic GA23-05377S, and National Institute for Cancer Research (EXCELES) LX22NPO5102.
Disclosures
Trněný:Gilead Sciences, Takeda, BMS, F. Hoffmann-La Roche Ltd, Janssen, AbbVie: Other: Travel, Accommodation, Expenses; Janssen, Gilead Sciences, Takeda, BMS, Amgen, AbbVie, F. Hoffmann-La Roche Ltd, MorphoSys, Novartis: Honoraria; Takeda, BMS, Incyte, AbbVie, Amgen, F. Hoffmann-La Roche Ltd, Gilead Sciences, Janssen, MorphoSys, Novartis, Genmab, SOBI: Consultancy. Klanova:Tubulis: Ended employment in the past 24 months.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal